Fertility and IVF: Transforming Hope into Parenthood
For many people, the path to parenthood isn’t always simple. Fertility challenges affect millions of couples worldwide, leading many to explore medical options like IVF (In Vitro Fertilization). Whether you’re just beginning to consider your fertility or are already exploring treatment options, understanding how fertility and IVF work can empower you to make informed decisions on your journey to becoming a parent.
In this guide, we’ll break down the basics of fertility, common challenges, and how IVF can offer hope when natural conception proves difficult.
Fertility: A Beautiful Beginning to Parenthood
Fertility refers to the natural ability to conceive a child. While many couples are able to conceive naturally within the first year of trying, around 1 in 6 couples experience difficulties—a condition referred to as infertility.
Key Factors That Affect Fertility:
- Age: Fertility declines significantly after age 35 in women.
- Ovulation disorders: Irregular or absent ovulation affects conception chances.
- Sperm health: Low sperm count or motility can hinder fertilization.
- Fallopian tube issues: Blockages can prevent egg and sperm from meeting.
- Endometriosis: Tissue growth outside the uterus can interfere with fertility.
- Lifestyle: Smoking, alcohol, obesity, and stress all negatively affect fertility.
Don’t Ignore the Signs: Seek Help for Infertility
. Here are key reasons to consider seeking professional guidance:
If you're under 35 and have been trying to conceive for a year without success, it's a good idea to consult a fertility expert. For those over 35, fertility naturally declines, and waiting too long could reduce the chances of successful treatment. In this case, seeking help after 6 months is recommended to avoid further delays.
A healthy, regular menstrual cycle is often a sign that ovulation is occurring properly. If your periods are irregular, too long, too short, or completely absent, it may indicate an underlying hormonal imbalance or ovulation disorder. Conditions like Polycystic Ovary Syndrome (PCOS), thyroid issues, or early menopause can interfere with ovulation and reduce fertility.
If either partner has a history of reproductive health problems—such as endometriosis, uterine fibroids, low sperm count, or past infections—consulting a specialist early is essential. A fertility expert can conduct thorough evaluations and suggest treatments tailored to your specific situation.
Recurrent pregnancy loss, typically defined as two or more consecutive miscarriages, can be emotionally devastating and may signal an underlying medical issue. A fertility specialist can help identify possible causes, such as genetic abnormalities, hormonal imbalances, or autoimmune disorders, and recommend treatment options to improve the chances of a successful pregnancy.
IVF: The Powerfull Possibility to Parenthood
In Vitro Fertilization (IVF) is an assisted reproductive technology (ART) that involves fertilizing an egg outside the body and then implanting the resulting embryo into the uterus.
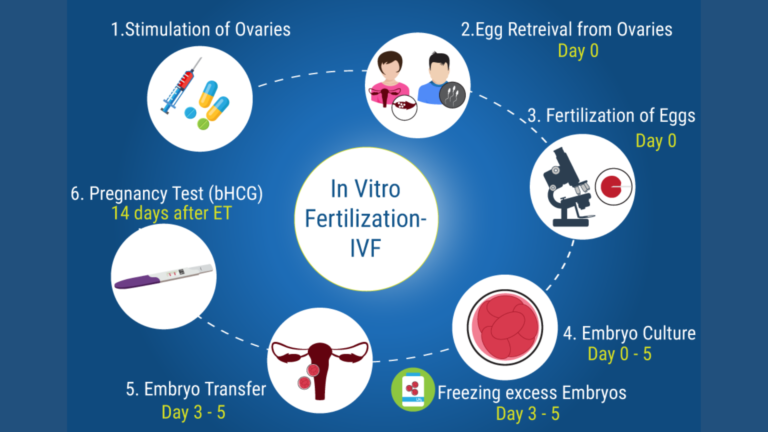
1. Ovarian Stimulation:
The IVF journey begins with ovarian stimulation, a phase designed to boost the ovaries into producing multiple mature eggs instead of the single egg typically released each month. Fertility medications, usually containing follicle-stimulating hormone (FSH) and luteinizing hormone (LH), are administered daily over a period of 8 to 14 days. During this time, doctors closely monitor the growth of ovarian follicles through regular ultrasounds and blood tests to track hormone levels and ensure the eggs are developing properly.
2. Egg Retrieval:
Once the follicles reach the desired size, a “trigger shot” is given to complete the eggs’ maturation. Around 36 hours later, the eggs are retrieved through a minor outpatient procedure called transvaginal ultrasound aspiration. Under light sedation, a thin needle is inserted through the vaginal wall into the ovaries to collect the eggs. This process typically lasts about 20–30 minutes and is followed by a short recovery period.
3. Fertilization
Following retrieval, the eggs are taken to the lab where they are fertilized with sperm from a partner or donor. There are two primary methods of fertilization: conventional IVF, where sperm and eggs are mixed together in a dish, and Intracytoplasmic Sperm Injection (ICSI), where a single sperm is directly injected into each egg, often used in cases of male infertility. The eggs are then monitored for signs of successful fertilization, which usually occurs within 24 hours.
4. Embryo Culture:
Once fertilized, the embryos are placed in an incubator to grow under controlled conditions. Over the next 3 to 5 days, embryologists observe the development of the embryos, watching for cell division and quality. By day 5, embryos may reach the blastocyst stage, a more advanced stage that often leads to better implantation rates. At this point, some clinics offer preimplantation genetic testing (PGT) to check for genetic or chromosomal abnormalities before selection for transfer.
5. Embryo Transfer:
One of the healthiest embryos is selected for transfer into the woman’s uterus. This is a painless and quick procedure performed without anesthesia. Using a thin, flexible catheter, the embryo is guided through the cervix and placed directly into the uterine lining. To increase the chances of successful implantation, progesterone supplements are often prescribed to support the endometrial lining during this critical phase.
6. Pregnancy Test:
Approximately 9 to 14 days after the embryo transfer, a blood test measuring beta hCG levels is performed to determine whether implantation was successful and pregnancy has begun. A positive test result confirms early pregnancy, while a negative result may lead to discussions about trying another cycle or exploring other fertility options. This final step closes the initial IVF cycle, offering either the joy of a positive result or insight into future reproductive planning.
Struggling with Infertility? Here’s Who Can Benefit from IVF
IVF is often recommended for individuals or couples facing:
Blocked or damaged fallopian tubes
Male infertility (low sperm count or quality)
Endometriosis
Unexplained infertility
Ovulation disorders
Genetic concerns (via preimplantation genetic testing)
Same-sex couples or single individuals using donor sperm or eggs
The Hidden Truth: Risks of Fertility Treatments You Must Know"
While generally safe and well-regulated, fertility treatments can have side effects or complications. Here are some of the most common:
Ovarian Hyperstimulation Syndrome (OHSS)
This can occur when the ovaries overreact to fertility drugs. Symptoms range from mild bloating to severe abdominal pain, nausea, and fluid accumulation.
Risk Level: Moderate
Treatment: Monitoring, fluid management, sometimes hospitalization
Multiple Pregnancies
Fertility treatments, especially IVF and ovulation-stimulating drugs, increase the chance of twins or higher-order multiples. While exciting for some, multiple pregnancies carry greater risks such as premature birth and low birth weight.
Risk Level: High (if multiple embryos are transferred)
Prevention: Elective single embryo transfer (eSET)
Emotional and Psychological Stress
The emotional toll of failed cycles, hormonal changes, physical discomfort, and the waiting game can be overwhelming. Couples often experience anxiety, depression, or relationship strain.
Risk Level: High for some
Support Tip: Consider counseling or joining a fertility support group
Side Effects from Medications
Fertility drugs may cause hot flashes, headaches, mood swings, and mild discomfort. Rare allergic reactions can also occur.
Risk Level: Low to moderate
Solution: Regular monitoring by your fertility doctor
Long-Term Health Uncertainty
While there’s no definitive link, some studies suggest a slight increase in the risk of ovarian or endometrial cancer with long-term use of fertility drugs, though the evidence is not conclusive.
Success Rates and Considerations
IVF success depends on several factors, including:
Age of the person providing the eggs (younger eggs tend to result in higher success)
Embryo quality
Uterine health
Lifestyle factors
Underlying medical conditions
Average IVF Success Rates:
Women under 35: ~40–50% success per cycle
Women 35–37: ~30–40%
Women 38–40: ~20–25%
Women 40+: ~10–15%
It’s important to remember that multiple cycles are sometimes necessary to achieve pregnancy.
Emotional and Financial Impact
IVF can be a physically and emotionally intense process. Hormonal treatments, the waiting, and uncertainty can be stressful. It’s essential to seek support from counselors, support groups, or fertility coaches.
In addition, IVF can be expensive, not including medications or additional procedures like ICSI or genetic testing. Some insurance plans offer partial coverage, and many clinics provide financing options.
Fertility and IVF go hand-in-hand when natural conception becomes a challenge. Thanks to incredible advances in reproductive medicine, IVF offers hope to millions of individuals and couples worldwide who dream of building a family. While the process can be complex and emotional, the success stories continue to grow.
If you’re facing fertility challenges, know that you’re not alone—and options like IVF can help turn your hopes into reality. With the right medical support, information, and emotional care, your path to parenthood is possible.
